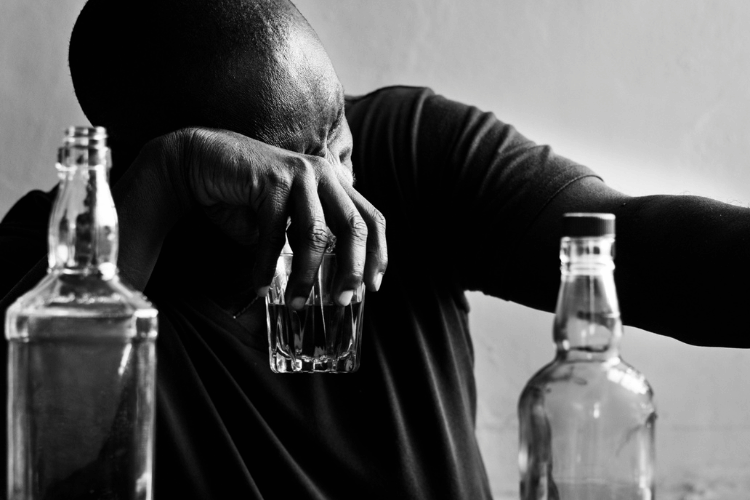
How to Stay Sober While Traveling or on Vacation
Traveling and vacationing can be exciting, but also testing times when trying to stay sober. It’s helpful to plan ahead and adopt strategies to help you stay on track with sobriety. Learning how to remain sober while traveling or having an enjoyable vacation without relying on alcohol or drugs is not difficult when you know how to find replacement activities and use your coping skills to address social pressure in tempting situations.
Avoid the Temptation to Drink and Use Drugs
The first step for staying sober while traveling or on vacation is recognizing and accepting that drinking alcohol or using drugs will not improve your experience but could ruin it. There will be times of stress and possibly boredom throughout any travel or vacation. However, it is essential to remember there are healthier ways of alleviating these feelings than using drugs or alcohol.
Prepare Different Strategies Ahead of Time
In order to keep on track with sobriety, there are many strategies you can employ when traveling or taking a vacation. For example, you should look up the schedule and location of support meetings in the city you will visit. Some resorts also offer onsite meetings, so you never have to leave the resort. It can also be beneficial to write a plan of what to do should you feel triggers and cravings coming on to make it easier during moments of temptation.
Assess Social Groups You Are With
Do some research before traveling or going on vacation, especially when traveling with a group. If alcohol or drugs will be present in various situations, assess what other activities you can get involved in or fill your time with instead. If you have business functions you need to attend, it is okay to make an appearance and leave early.
Drink Mocktails
Mocktails are a great way to make it appear like you are drinking, even though you are sticking to non-alcoholic alternatives. This will alleviate peer pressure from family, friends, or co-workers who do not fully understand addiction and insistence you have one drink.
Utilize Resources from Aftercare Programs
Make sure to take contact information for your at-home aftercare support with you when traveling or going on vacation. Being able to connect with people from your program, who understand your struggles, can provide encouragement and can help keep you motivated during moments of difficulty.
In addition, explore aftercare support options available in the location where you will be traveling. Many programs can refer you to local meetings and contacts that can benefit your sobriety when away from home.
Consider Sober Travel Groups
Sober travel groups are growing, especially with the increase of online platforms. Consider traveling in a group that explicitly promotes sobriety to help you remain encouraged and supportive throughout a vacation or when away from home on business.
Avoid Situations and Places That Could Tempt You
By avoiding situations and spaces that could lead to giving in to temptation, many people are able to remain on track with sobriety while traveling or on vacation. If you have to travel to a location well known for having a partying atmosphere, see if there’s any easy way of staying elsewhere. For example, consider booking a vacation rental home in a residential area further away from all that commotion.
Remember Techniques Learned in Support Groups or Therapy
Reflecting on any techniques learned from support groups or therapy that encouraged your sobriety is also beneficial. Utilizing these techniques while traveling can help alleviate stress and anxiety when faced with tempting environments.
Remember Your Self-Care
It is also important to maintain self-care while traveling or on vacation. This doesn’t necessarily mean always sticking to your established routine. However, remember to eat balanced meals and spend some time in the fitness center.
Your travel or vacation self-care could also include the following:
- Exploring activities where drugs and alcohol are not present.
- Doing the things that bring you pleasure.
- Having some flexibility to adjust your schedule as needed to mediate or have some downtime for personal reflection.
Take Advantage of Online Support
Thanks to technology, you have access to different online support options to remain sober while traveling or on vacation. You can find online group meetings or connect with your at-home therapist or sponsor. Some aftercare support programs also have telehealth options, so you can join your regular meetings even though you are not home.
Conclusion
Staying sober while traveling or on vacation may seem like a daunting task. However, there are several strategies one can employ to remain true to their commitment. Whether enlisting friend support and creating positive distractions or avoiding triggering environments all together, one’s mindset is essential for achieving success over temptation, remaining sober while traveling, and having an enjoyable stay away from home.
Aftercare, Travel, and Vacation Support in Murfreesboro, TN
At Tulip Hill Recovery in Murfreesboro, TN, we want you to maintain your sobriety when traveling or on vacation. We provide access to resources and aftercare to ensure you receive the care and support you need when away from home. Contact us today for further information.